Dental pulp precursors
Indicated as a therapeutic complement in regenerative dentistry and oral-maxillofacial surgery procedures, under the protocol and criteria of the specialist.
Presentation and concentration

Mechanism and evidence
Paracrine and immunomodulation: secretion of extracellular factors and vesicles that modulate inflammation and stimulate tissue repair.
Odontogenic and osseous potential: capacity of differentiation towards lineages odontoblast y osteogenicwith better performance when combined with biocompatible scaffolds.
Regenerative endodontics: evidence in development; experimental protocols with variable results.
Periodontics and implants: support in intrabony defects, alveolar ridge preservation y integration with biomaterials (early clinical phase).
Origin and method
Source: dental pulp of third molar o healthy deciduous toothobtained under planned extraction and clinical screening.
Isolation and expansion: made under controlled conditions of sterility.
Characterization and quality
Mesenchymal identity (ISCT criteria): adhesion to plastic; positive for CD73⁺/CD90⁺/CD105⁺/CD105⁺negative for CD14/CD19/CD34/CD45/HLA-DR.
Feasibility and count: determined by flow cytometry (7-AAD/PI) with standardized analysis.
Microbiology and safety: sterility (USP), mycoplasma (qPCR) and endotoxins (LAL).
Transparency: the cryopreservation may influence feasibility; acceptable ranges and time of measurement are stated in the technical documentation.
Use and preparation
Local application: at root canals, intrabony defects o alveolar bone areasin combination with biomaterials (collagen, HA, β-TCP, hydrogels).
Indicative dosage: 25 million cellsadjusted to the size of the defect and the specialist's criteria.
Technique: thawing under control, mix gently with the chosen biomaterial and apply immediately.
Conservation and logistics
Storage: keep between 2-8 °C to its application.
Cold chain: do not administer if it is interrupted or if they have passed >72 h since shipment.
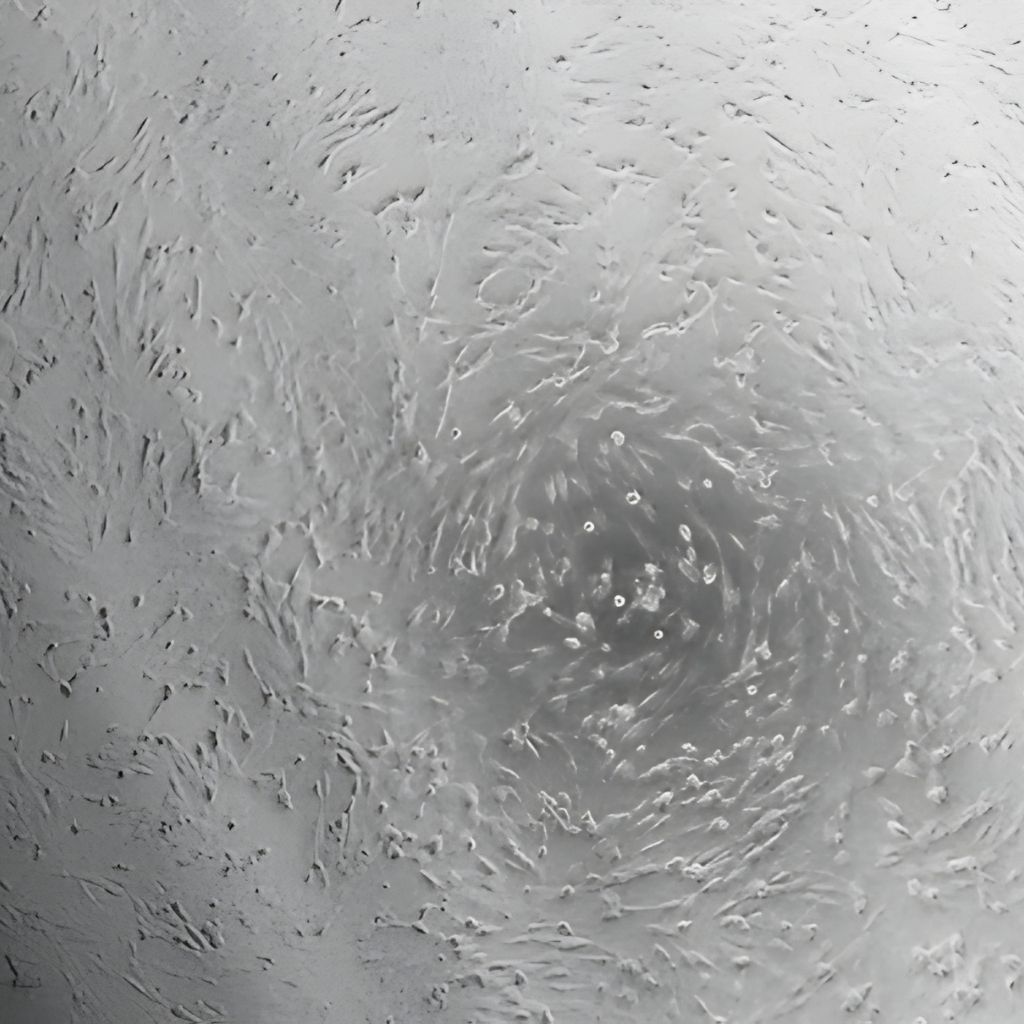
What are dental pulp precursors (DPSC)?
Stem cells mesenchymal derived from pulp tissuea vascular and innervated tissue with high proliferative and multipotent capacity.
They can be differentiated towards odontoblasts, osteoblasts, chondrocytes, chondrocytes and even lineages neuroectodermal in research.
In dentistry, the DPSCs are used as therapeutic adjunct in procedures for regenerative dentistry, advanced endodontics, periodontics y oromaxillofacial surgerywhere they favor the dentin-osseous tissue neoformation and the integration with biomaterials.
The clinical evidence is promisingIndications and dosages must be defined case by caseaccording to the extent of the defect and the specialist's criteria.
Guided periodontal regeneration (GTR)
Guided periodontal regeneration (GTR)
They promote the reconstruction of the periodontal ligament and the alveolar bone, favoring the functional reinsertion and stability of the dental support.
Alveolar preservation post-extraction
They contribute to preserving the alveolar volume and architecture after tooth extraction, reducing resorption and facilitating subsequent implants or prostheses.
Guided Bone Regeneration (GBR)
Biological support in horizontal or vertical bone augmentation procedures; combined with barriers and scaffolds to stimulate more predictable osteogenesis.
Maxillary sinus lift
They accelerate the formation of new bone within the maxillary sinus when associated with grafting materials or osteoconductive matrices.
Our biotechnology products

Stromal Precursors (MSC)
10 Million
25 Million
50 Million
Mechanism and evidence
Paracrine and immunomodulation: factors and EV that adjust inflammation and promote repair.
Odontogenic/bony potential: differentiation odontoblast-like and bone; better performance with scaffolding adequate.
Regenerative endodontics: evolving protocols; results heterogeneous between studies.
Periodontium/implants: support in intrabony defects and ridge preservation (early evidence).

Natural Killer (NK) Cells
25 Million
50 Million
Mechanism and evidence
Direct cytotoxicity: cell recognition with MHC-I low/absent and lysis by perforin/granzymes.
ADCC (CD16): synergy with monoclonal antibodiesdestroys cells opsonized with IgG.
Immunoregulation: secretion of IFN-γ/TNF-α y crosstalk with dendritic and Tadjusting the tumor microenvironment.
Evidence framework: mechanisms valid in basic immunology; ongoing clinical translationwith response influenced by patient status, KIR/HLA profile and degree of activation ex vivo.
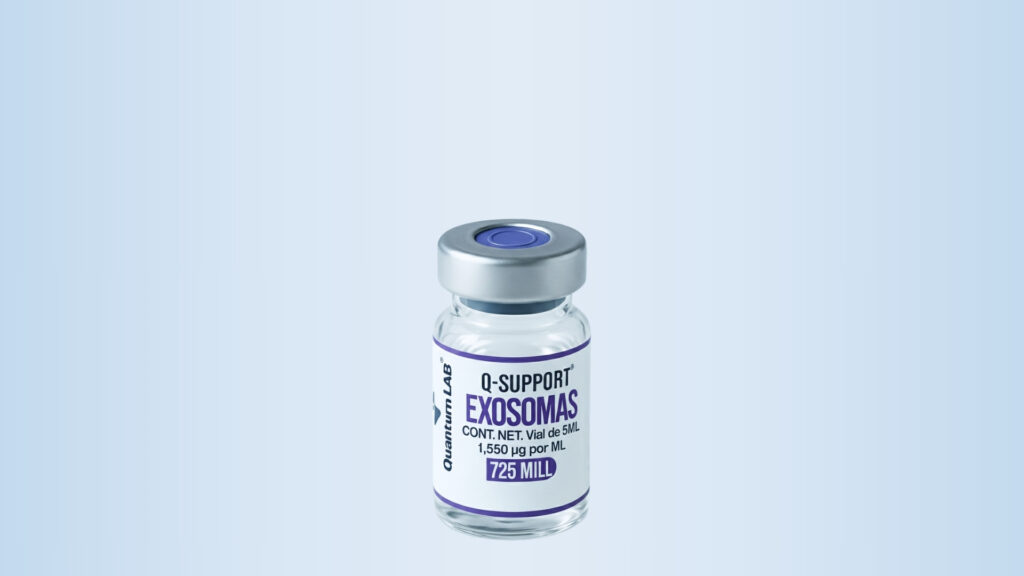
Exosomes
1,550 µg per vial of 5 mL
Mechanism and evidence
They act as natural mediators of cellular communication, transferring proteins, RNA and bioactive factors that modulate the inflammatory response and stimulate endogenous regeneration mechanisms.
Promote the controlled angiogenesisthe reorganization of the extracellular matrix and the functional recovery of tissuereducing variability in clinical outcomes and return-to-work times.
Developed for scenarios where predictable recovery, pain reduction y sustained tissue stability during follow-up.
